Rose* was 30 when she had her first Pap smear, a routine test for women that screens the cervix for any abnormalities. It was on her "to-do list" that marked her entry into a new era of adulthood, right next to "go to the dentist" and "save money". "I'd been wanting to do it for at least a year but kept putting it off," the Iraqi sales manager who lives in Dubai tells The National. "Turning 30 gave me the push I needed."
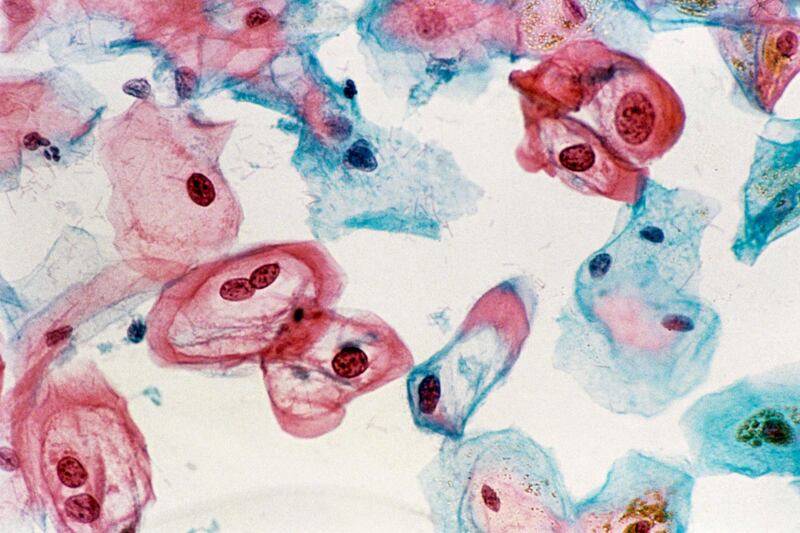
When she did finally make it to the gynaecologist, she was told she had human papillomavirus (HPV), a sexually transmitted group of cancer-causing viruses she’d only recently learnt of. “I’d heard of HPV because my friend had had it, but she had a mild strain, so she’d spoken about it in a very casual way,” Rose explains. “I didn’t think it was a big deal.” After the initial test, she was called back for a biopsy, and then told she’d need to have surgery as they’d discovered two aggressive strains of the virus on her cervix. That’s when she began to panic. “I literally thought I had cancer and could die, and that hit me hard. I was really shocked and upset.”
At the same time, Annabel*, a British expat who also lives in Dubai, was going through a similar experience. The 27-year-old had her Pap smear quite by accident, as part of a more general check-up, and found she also had a high-risk strain of HPV, something she’d never heard of before. “I just forgot about [having the test],” she admits. “In England, you get a letter from the National Health Service reminding you to go, but here, I didn’t even think about it.” She ended up going through a four-month process of tests and surgery, which saw her visit three different doctors across two emirates, before being given the all-clear.
A mountain of misconceptions
Both Rose’s and Annabel’s stories highlight some of the most prevalent misconceptions surrounding Pap smears, HPV and cervical cancer among women today. Often, if they don’t already know what HPV is, they don’t understand how important it is to get regularly checked. If they have, many ladies fear a positive result showing abnormal cells is a fast-track to a cancer diagnosis. But that’s just not the case.
“This virus is extremely common,” Dr Aagje Bais, a consultant obstetrician and gynaecologist at Dubai’s Mediclinic Arabian Ranches, explains. “Eighty per cent of all people, females and males, will get it once in their lifetime.
“I compare it with the flu – almost everyone gets the flu at least once, only with the flu you’re sick, you have a fever and you have to lay in bed. With [HPV] you don’t know you have it,” she explains.
There are more than 100 types of HPV, of which at least 14 are cancer-causing (also known as "high-risk" or "high-grade"), according to the World Health Organisation. The virus causes about 99.9 per cent of cervical cancers, and because it takes a long time to progress, it's a very preventable disease. Alongside regular screenings for early detection, which has resulted in a five-year survival rate close to 96 per cent, there's also an HPV vaccine, available for children aged 13 and up, which has shown to be highly effective in preventing infection from some of the most common strains of the virus. In fact, new research published in the journal Lancet Oncology shows how scaling up vaccine coverage and screening could effectively eliminate cervical cancer all together.
Yet, despite these optimistic figures, in the UAE, 1.9 million women are at risk of developing cervical cancer, according to the Human Papillomavirus Information Centre of the Catalan Institute of Oncology and the International Agency for Research on Cancer.
“This is what we want to prevent,” says Dr Suhaila Alameeri, a consultant anatomic pathologist at the National Reference Laboratory and a member of the National Taskforce for Breast and Cervical Cancer Screening programme. The Emirati doctor emphasises Dr Bais’s point: “It’s a common infection, and most women won’t have cancer. Usually it’s cleared up by the body, but a few per cent of patients will progress through legions.” If you’re diagnosed with high-risk HPV, like Rose and Annabel were, you’ll most likely need to have laser surgery in order to remove the cells.
It might take decades for these cells to morph into cancer, but finding them in the first place is key, as there’s no way of telling how long they’ve been in your body, Dr Bais explains. “You can have HPV and it can be present for a long time, many years sometimes, and it can be there, doing nothing, and suddenly it becomes active, then it will change the cells on your cervix and give you an abnormal Pap smear. At that time, your own immune system is activated to start to get rid of this virus. When the virus is gone, your Pap smear will turn back to normal. That’s what usually happens.” So there’s plenty of time to detect any changes on your cervix at the pre-cancerous stage, adds Dr Alameeri. “Then we can treat the patient and prevent cancer.”
But that’s only if you go to the gynecologist in the first place.
When to get checked
The Department of Health Abu Dhabi has recently updated its Guidelines for Cervical Cancer Screening. They recommend that all females aged 25 to 29 undergo a Pap smear every three years, while women aged 30 to 65 should do both a Pap smear and HPV test every five years (a Pap smear detects the presence of abnormal cells that could indicate cancer, while the latter only shows HPV).
These age guidelines may not always be relevant, however, warns Dr Alameeri. “If a woman is sexually active, she has to start cervical cancer screenings. This is the bottom line.” This includes women who have been the subject of sexual abuse.
With no population-based screening programme, like they have in Dr Bais’s native Netherlands, women may not realise they need to have a smear test, or they’ll simply forget to book an appointment, like Annabel did. “Not all females are aware of the possibility and options of having a Pap smear,” says Dr Bais. “And also the necessity – people think that because they don’t have [symptoms] they’ll be fine.” Unfortunately, with cervical cancer, patients don’t show symptoms, such as unusual vaginal bleeding and increased discharge, until it’s already too late, she explains. “The good thing is we can detect these minor abnormalities, these minor changes, and keep an eye on it.”
Among other reasons, Rose says she also put off booking her appointment because she was worried about not feeling comfortable with her doctor. Leila*, a 28-year-old Jordanian based in Dubai, admits that, for her, it was more a mixture of fear and laziness. “I know it’s stupid, but you put it off, time flies. I think women our age or in general go to the gynecologist when they’re worried about an STD [sexually transmitted disease] rather than going to get checked for cancer or anything like that. I wasn’t worried about that, so maybe that’s why I didn’t care to go.”
An issue of education?
Ultimately, whether we're talking about vaccinations or smear tests or HPV itself, there is so much misinformation and ignorance surrounding topics of female sexual health across the world – not just here in the UAE. Sarah*, a 32-year-old Canadian-Lebanese woman, says she thinks we need to start learning about it all from a younger age. "I didn't start doing the test until after I was 25," she tells The National. "I come from a culture where our parents don't talk about this or sexuality or anything like that. It was definitely a taboo. I had no guidance.
“Schools in Lebanon only talked about our period and that was it. Biology classes never talked about females and how they grow and what needs to be done. In Canada, I remember the doctor asking when my mum was with me, if I wanted to be alone in the room. Obviously I wasn’t going to ask her to leave – it’s a culture and respect thing.
“It’s a bit complicated, so I never knew what it [a Pap smear] was until I started talking to girlfriends who do the test and understanding why they do it.”
Rose, who was brought up in Dubai and attended schools in the UAE, also believes this lack of female-focused education needs to be addressed. “I really think it needs to be spoken about more and normalised,” she says.
In the UAE, sex education is not compulsory. At Jumeirah English Speaking School (Jess) Dubai, for example, there are no talks given to schoolchildren on the topic of Pap smears. "The general medical guidance on Pap smears is that they are only conducted over the age of 25 and our eldest students are only 18 years old," Jess Dubai director Mark Steed confirms. "We do offer puberty talks to our Year 6 children who are 11 years of age. In these talks, which are run by our nurses and staff, boys and girls are taught separately about the physical changes they can expect in their body as they approach puberty.
“We [also] offer a question-and-answer box where children can write anonymous questions that our nurses and staff answer.” Yet, he adds, parents are advised of the content of these lessons in advance, and they can choose for their children to opt in or out of these talks.
A source of shame
It’s particularly telling that everyone we interviewed for this article asked to remain anonymous. Admitting you’ve had HPV and simply talking about Pap smears so publicly can be a source of embarrassment and shame for women everywhere. “There’s a lot of psychological trauma around it,” Dr Alameeri says. “Some patients won’t even tell their partners or family about this infection.”
Dr Bais has seen the same attitude among her patients. “I think because HPV is a sexually transmitted virus, it is a major burden for some people. They say ‘is it like an STD?’ To be honest, no, not really, but it is sexually transmitted.
“If it’s your first partner and you’ve never had any other sexual partner, and they haven’t either, then of course you won’t have HPV, but this is so unlikely.
“It’s a delicate subject, of course it is … [But] we’re not talking about STDs, we’re just going to see if there’s any abnormality.”
Dr Alameeri agrees that approaching the subject in this way can begin to break down any barriers. “We need to listen to the patients, understand the myths the patients believe, and then bust that myth with evidence-based information.”
Misconceptions surrounding the vaccine abound, too, as the number of people who are anti vaccinations rises. Dr Mai Ahmed Sultan Al Jaber, an Emirati medical director and public health medicine specialist at Healthpoint, stresses the importance of girls getting vaccinated when they’re still young. “We have to convince people vaccines are safe – they are tested and have been through several trials to be recognised and approved.”
Dr Bais also stresses this point. “All of the stories about becoming infertile, getting autism, people dying, getting cancer [from the vaccination], it’s all not true. It’s not related. It has a bad reputation, but it’s scientifically proven that it’s not true. It’s a safe thing to use.”
This is a growing issue the government has also added to its national agenda. In a February forum in Sharjah, called “Turning the Tide on HPV and Cervical Cancer”, Dr Laila Hussen Al Jasmi, head of immunisation at the Ministry of Health and Prevention, announced schoolgirls aged 13 and 14 across Dubai and the Northern Emirates will get their first dose in March. “Starting from next academic year, the vaccine will become a routine procedure,” she said. In Abu Dhabi, it’s already compulsory under the emirate’s vaccination programme.
Don’t let life get in the way
One of the biggest hurdles for women getting checked is a busy schedule, says Dr Alameeri. This is particularly prevalent among mothers, who often put their family first, she adds. “I want to tell them: love yourself, you have one body, so love your body like you love your family. Go for a test. There is nothing to fear, there’s no shame, it’s a very common infection.”
If you don’t, and your abnormal cells progress, it’s much more difficult to treat, warns Dr Bais. “People still die of cervical cancer. What we see is that more than 50 per cent of people who develop cervical cancer – when it’s too late already – didn’t have a screening done. We have an easy way to prevent that, just to keep an eye on it.”
Rose, for one, has certainly learnt her lesson. “It’s a necessary test every woman needs to do,” she says. “It’s not scary. It’s not painful. Yes, it’s a little uncomfortable, but it needs to be done.
“Do your research, talk to your friends – most likely everyone will have their own story – and find a doctor you feel comfortable with. Regular check-ups are so important.”
After all, it’s just a matter of being uncomfortable for two minutes to prevent years of suffering, says Annabel. “We’re so lucky that we have this test available to us. There are some types of cancers and health issues that there are no screenings for. With this, we can get it checked and fixed before it even turns into cancer. You have the opportunity to save your own life, so do it.”
Names and some personal details have been changed to protect privacy