Diabetes, the chronic health condition characterised by the body’s inability to regulate blood glucose levels, is becoming more prevalent.
It is linked to blindness, kidney failure, heart attacks, strokes and amputation.
World Diabetes Day is observed annually on November 14. For those living with diabetes, the body either doesn’t produce enough insulin or can’t use it effectively, leading to various health challenges.
But with appropriate knowledge and management, those with the condition can lead full and active lives.
The International Diabetes Federation (IDF) Diabetes Atlas (2021) reports that 10.5 per cent of the adult population (20-79 years) has diabetes, with almost half unaware that they are living with the condition.
By 2045, IDF projections show that one in eight adults, approximately 783 million, will be living with diabetes, an increase of 46 per cent.
According to recent statistics, an estimated 537 million adults globally are living with diabetes, expected to rise to 643 million by 2030.
Insulin's role in diabetes
Insulin, a vital hormone produced by the pancreas, plays a crucial role in regulating blood sugar levels. It enables the movement of glucose from the bloodstream into the body's cells, where it is transformed into energy or stored for later use.
Insulin is also essential for the metabolism of proteins and fats. When there is a deficiency of insulin or when cells are resistant to its effects, blood glucose levels rise significantly, leading to hyperglycaemia, the primary clinical indicator of diabetes.
An unchecked insulin deficit over an extended period can lead to severe and potentially life-threatening health complications. These include cardiovascular diseases, nerve damage, kidney damage, lower-limb amputation and eye diseases, particularly those affecting the retina, which can lead to loss of vision and blindness.
With proper management, the onset of these severe complications can be delayed or even prevented.
Types of diabetes
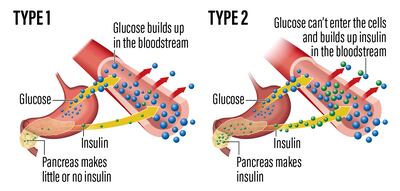
Type 1 Diabetes is an autoimmune condition where the body's immune system attacks and destroys the insulin-producing cells in the pancreas. It is often diagnosed in childhood or young adulthood but can occur at any age. Unlike other types, it is not related to lifestyle factors and is less common than Type 2. The exact causes are not fully understood, but genetic factors and environmental triggers such as viruses may play a role.
Type 2 diabetes is more prevalent and typically develops in adults, although it's increasingly seen in children and adolescents. This type occurs when the body becomes resistant to insulin or when the pancreas cannot produce enough insulin. Risk factors include obesity, physical inactivity, poor diet, advancing age and family history. Unlike Type 1, lifestyle factors play a significant role in the development of Type 2, making it more common.
Gestational diabetes occurs during pregnancy and usually resolves after childbirth. However, it increases the risk of developing Type 2 diabetes in the future for mother and child. It is diagnosed through prenatal screening and is managed by monitoring blood glucose levels, diet and exercise. In some cases, medication is needed.
Other less common variants include Latent Autoimmune Diabetes in Adults (Lada) and Maturity-Onset Diabetes of the Young (Mody). Lada is a form of Type 1 that develops slowly and typically appears in adulthood, often being misdiagnosed as Type 2. Mody is a rare form caused by a mutation in a single gene, affecting insulin production. Other rare forms of diabetes can result from specific genetic syndromes, surgery, drugs, malnutrition, infections and other illnesses.
Signs and symptoms
Common symptoms shared by both Type 1 and Type 2 include an intense feeling of thirst and an increased need to urinate. These symptoms are due to the excess glucose in the bloodstream, which the kidneys attempt to filter and excrete in urine, requiring more fluid intake.
Other shared symptoms are blurred vision, tiredness and unintentional weight loss. The weight loss in diabetes occurs as the body starts to break down fat and muscle for energy due to its inability to properly use glucose without adequate insulin.
While many symptoms are shared between types 1 and 2, they can vary in their onset and severity. In Type 1, symptoms often appear suddenly and are more severe, whereas Type 2 symptoms can be mild and develop gradually, sometimes taking years to be noticed. This gradual onset can delay diagnosis and treatment, leading to more significant damage over time.
Diagnosis
Diagnosis of diabetes is primarily based on blood tests. The main tests used are the fasting plasma glucose, the oral glucose tolerance and the HbA1c.
The fasting plasma glucose test measures blood sugar levels after an overnight fast.
The oral glucose tolerance test involves fasting overnight, having blood sugar level measured, drinking a sugary liquid and then having blood sugar levels checked several times over the next two hours.
The HbA1c test, also known as the A1c or glycated haemoglobin test, measures the average blood sugar levels over the past two to three months.
The criteria for diagnosis are strict to ensure accuracy. These tests help distinguish between different types of diabetes and prediabetes, a condition where blood sugar levels are high but not high enough to be classified as diabetes.

Management and treatment
The focus is on controlling blood sugar levels to prevent complications. A combination of lifestyle changes, medication and regular monitoring is often necessary.
Lifestyle changes, particularly in diet and exercise, are fundamental in managing diabetes. A healthy diet rich in fruit, vegetables, whole grains and lean proteins helps control blood sugar levels. Reducing intake of sugars and refined carbohydrates is also crucial. Regular physical activity helps maintain a healthy weight and improves insulin sensitivity, making it easier for the body to regulate blood sugar levels.
Medication is a key component of diabetes management. Oral medication, such as metformin, is commonly prescribed for Type 2 to help improve insulin sensitivity and reduce glucose production in the liver. For Type 1 and sometimes Type 2, insulin therapy is essential. Insulin is administered through injections or a pump to regulate blood sugar levels. The type and dosage of medication depend on the patient's specific needs and the type of the condition.
Monitoring blood sugar levels is vital for people with diabetes. Regular testing allows for adjustments in diet, exercise and medication to maintain blood sugar within a target range. This monitoring can be done at home with a blood glucose meter or continuous glucose monitoring systems.
Complications of diabetes
Diabetes can lead to a range of complications if not managed properly, with significant effects on health and quality of life.
Short-term complications include hypoglycaemia, hyperglycaemia and diabetic ketoacidosis.
Long-term complications are typically the result of prolonged high blood sugar levels and can develop over several years. They include cardiovascular disease, which is more common and more severe in people with diabetes, leading to an increased risk of heart attacks and strokes.
Living with diabetes
Living with diabetes involves adapting to a daily routine centred around diabetes care, managing the psychological aspect of the condition and using support systems.
Daily routines for people with diabetes typically include regular blood sugar monitoring, adhering to a balanced diet, maintaining physical activity and taking medication as prescribed. This routine requires careful planning, especially around meals and physical activities, to ensure blood sugar levels stay within target ranges.
The psychological impact of living with a chronic condition such as diabetes can be telling. People may experience stress, anxiety or depression related to continuing management and worry about potential complications. Coping with these emotional aspects is crucial for overall well-being. This can include seeking professional mental health support, practising stress-reduction techniques such as mindfulness or meditation, and staying informed about the condition to feel more in control.

Prevention and risk reduction
Lifestyle changes can significantly reduce the risk of developing Type 2 diabetes. This includes adopting a healthy diet rich in fruits, vegetables, whole grains and lean proteins, while minimising processed foods and sugars. Regular exercise is also crucial; it helps manage weight, improves insulin sensitivity and lowers blood sugar levels. Weight management is another key factor; maintaining a healthy weight reduces the risk of diabetes and improves overall health.
Impaired glucose tolerance (IGT) and impaired fasting glycaemia (IFG) are pre-diabetic states.
IGT is characterised by higher than normal blood sugar levels following meals, while IFG is indicated by higher than normal blood sugar levels after fasting. Both are intermediate conditions in the transition from normal glucose tolerance to diabetes and signal a heightened risk for developing Type 2. However, progression to diabetes is not inevitable.
People with IGT or IFG can often prevent the progression to diabetes through lifestyle modifications.
For women with gestational diabetes, careful monitoring and management during pregnancy are crucial.
Prevention strategies are particularly important in high-risk populations, such as those with a family history of diabetes, certain ethnicities with higher predisposition and people with obesity. Regular screening for diabetes in these groups can help with early detection and intervention.

Advancements in diabetes care
Building on the existing advancements in diabetes care, researchers are making significant strides in developing new treatments and medications.
GLP-1 receptor agonists represent a major advancement in diabetes treatment. This medication works by replicating the effects of the naturally occurring hormone GLP-1, which helps lower blood sugar by stimulating insulin production and inhibiting glucagon production. They have proven effective in not only lowering blood sugar levels but also in reducing cardiovascular complications in individuals with Type 2.
SGLT2 inhibitors are another class of medication making a notable impact. They function by blocking the SGLT2 transporter in the kidneys, responsible for reabsorbing glucose back into the bloodstream. By inhibiting this transporter, these drugs increase the excretion of glucose in urine, thereby lowering blood sugar levels and also reducing cardiovascular risks in people with Type 2.
Amylin mimetics imitate the hormone amylin, which is co-secreted with insulin and helps reduce post-meal blood sugar spikes by slowing gastric emptying. They have shown effectiveness in controlling blood sugar levels and decreasing the risk of cardiovascular issues in Type 2.
Technological advancements, particularly insulin pumps and continuous glucose monitors (CGMs) have revolutionised diabetes management.
Insulin pumps provide continuous insulin delivery, customisable to the user's needs, leading to more stable blood sugar levels. CGMs offer real-time blood sugar monitoring, allowing users to track their glucose levels throughout the day, recognise patterns and adjust insulin doses, dietary habits and physical activity accordingly.
Islet cell and stem cell studies are particularly promising. Efforts are continuing to transplant islet cells into individuals with Type 1 to restore insulin production. Similarly, there is significant research in developing stem cells into islet cells for transplantation, potentially offering new treatment avenues for Type 1.







