A report has found that standards of infection prevention and control (IPC) in UK hospitals have dropped since the pandemic.
The Royal College of Emergency Medicine recommended that IPC be put at the top of hospitals' agendas or patients’ lives could be at risk, with staff and patients still able to contract Covid-19.
The report recommended healthcare workers get vaccinated against the virus and have their flu injections.
The three-year quality improvement programme by the college gathered data on more than 65,000 patients across 127 emergency departments.
The report investigated the level of screening across three categories, including tests for Covid-19.
It also examined screening in those with "vulnerable conditions", such as being pregnant, unvaccinated or having immune system problems, and patients presenting with symptoms such as diarrhoea, vomiting or unexplained rash and fever.
The report found the national average of patients being screened when attending A&E was 17 per cent last year, down from 25 per cent in 2022.
"It is unconscionable that directly after a terrible pandemic the system is not providing the standards that staff and patients need," Royal College of Emergency Medicine president Dr Adrian Boyle said.
"We must ensure that an environment where staff and patients are protected properly against infectious diseases is the norm."
More than a quarter of emergency departments – 35 of the 127 surveyed – did not record any patients being screened for all three conditions.
The report warned there had been a "rise" in patients going into emergency departments with Covid-19, as well as a drop in the number of healthcare staff being vaccinated against the virus and flu.
"It is unclear why this is happening but we have an increasingly concerning situation for both patients and staff," the report added.
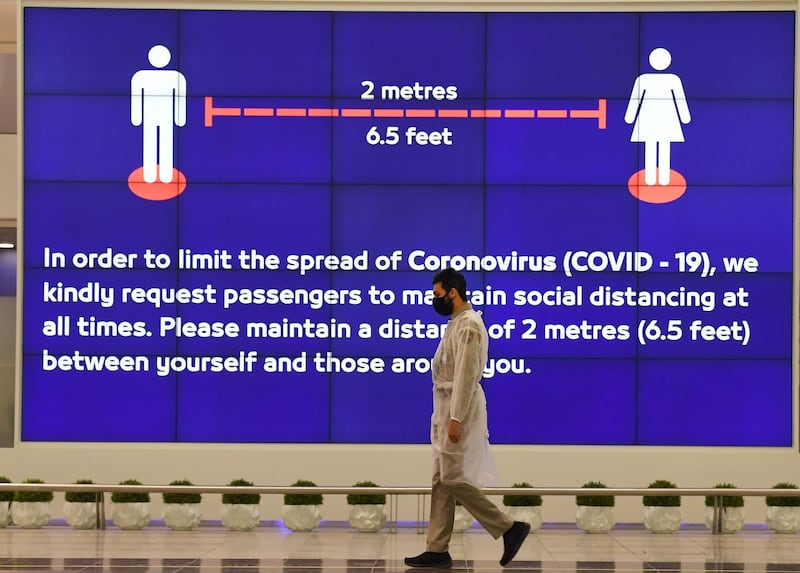
Anniversary of first Covid-19 death - in pictures
Elsewhere, the college found the national average of patients identified as potentially infectious and moved to an appropriate area was 62 per cent, down from 80 per cent.
On average, those patients were moved in 135 minutes, up from 83 minutes in the previous 12 months and 46 minutes in 2020-2021.
In his foreword, Dr Boyle wrote that the results show "performance has dropped across all the QIP's standards".
"In some instances, performance has dropped by over 20 per cent across the three years, highlighting the need for trusts and hospitals to return to placing IPC [infection prevention and control] at the top of their agendas as was done in the Covid-19 pandemic."
Among its recommendations, the college said: "We must continue to raise awareness that Covid-19 is present and a real risk to both patients and staff."
It called for staff to be "encouraged" to screen patients and document results, as well as to get vaccinated.
It also said IPC teams must work with emergency departments to maximise patient safety.
The college's QIP team was led by Dr Fiona Burton, an emergency medicine consultant.
Impact of the Covid-19 pandemic will be felt for 'decades to come' - video
Impact of the Covid-19 pandemic will be felt for 'decades to come'

She said the drop in standards was "worrying" but that the "highly unusual context" of the pandemic, as well as overstretched emergency departments, had to be considered.
"As Covid emerged there was naturally strong messaging about the importance of escalating infection control measures, including the focus on identifying the people who were most vulnerable," Dr Burton said.
"However, with the successful vaccination programme the messaging has lessened and assessing people's vulnerability as soon as they enter the emergency department is perhaps no longer as prominent a consideration as it was – especially as other system pressures mount.
"But we have to remember that Covid has not gone away and it, and other infectious diseases, still pose a serious threat to patients and to staff, and that not being able to provide adequate IPC measures can put people's lives at risk. It must remain a priority."
Publication of the report comes after health chiefs warned the National Health Service in England is facing an enormous challenge due to winter pressures and industrial action by junior doctors, which started on Saturday.
Data released last week showed an average of 2,208 patients were in hospital in England each day last week with flu, including 112 in critical care beds.
The figure is up by 68 per cent compared to the start of January, while the number in critical care is the highest so far this winter.
An average of 2,720 people who had tested positive for Covid-19 were also in hospital last week, down from 3,229 the previous week.
Covid-19 patient numbers peaked at more than 9,000 last winter.
An NHS representative told PA that NHS teams were "very aware" of the continuing risk presented by Covid-19 and "other infections", adding that "strong" prevention and control methods were already in place.
"The NHS urgent and emergency care recovery plan sets out a range of measures to reduce pressure and crowding in A&E, including greater use of community and same-day emergency care, alongside more beds and measures to reduce delayed discharges which affect patient flow and how quickly someone can be admitted,'" the representative said.
Agencies contributed to this report.