DUBAI // They are the pride of Arabia, the ships of the desert. Noble beasts, they change hands for millions of dirhams and are prized for their beauty. Now, according to scientists, camels could hold the key to a better cure for some of the world's deadliest snakebites.
A collaboration between researchers from Britain and Dubai using camels instead of the usual horses or sheep as incubators for a new antivenom is entering its final stages. The project is focusing on African snakes including the puff adder, the saw-scaled viper and the black spitting cobra, which between them kill up to 30,000 people a year. Antivenom is produced by injecting small amounts of toxin into animals and then harvesting antibodies, the proteins produced by the immune system to fight viruses, bacteria and venom. It is these antibodies, in serum form, that allow a person who has been bitten to fight the venom.
Because of the harsh environment in which camels live, they produce better antibodies than horses and sheep, according to Dr Ulrich Wernery, the scientific director of the Central Veterinary Research Laboratory (CVRL) in Dubai. Current antivenoms need to be kept frozen, a major stumbling block in parts of Africa, where unreliable electricity supplies give the treatments a short shelf life. This contributes to their high cost, putting the cures beyond the budgets of doctors in many areas where they are most needed. With few customers for antivenoms, big pharmaceutical companies largely halted production a decade ago.
Camel antibodies, however, are more resistant to heat, so the new antivenom should not need to be kept frozen. "This is very important for Africa," Dr Wernery said. The antibodies produced by camels are also much smaller, about one-tenth the size of those from horses or sheep, so they penetrate tissues far more easily. The team also hopes that the camel antivenom will provoke fewer allergic reactions.
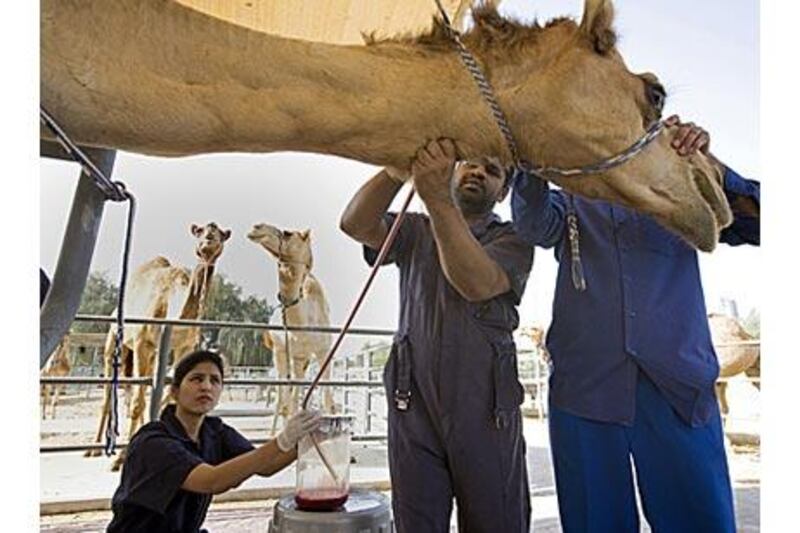
CVRL is collaborating with scientists from the Liverpool School of Tropical Medicine, which has been collecting venom from many of the world's most poisonous snakes. In Dubai, the CVRL team has injected each of about 40 camels with tiny amounts of the toxins from the African snakes. "We regularly take blood and check if the level of antibodies is high enough," Dr Wernery said. Each week, he collects 250 millilitres of blood from each camel to test whether the animal has started to produce antibodies.
Once the level of antibody production peaks, more blood is collected. Yesterday, "6A5", a five-year-old male camel of the local breed, had reached that peak. It was led away from its enclosure, into a specially designed stand. There, Dr Wernery shaved a small area on the left side of its neck, revealing a vein as wide as a child's hand. He made a small incision into the vein and inserted a large needle to collect the blood, which trickled into a large glass jar.
Once collected, the blood is left at room temperature for up to six hours so that the serum, the part of blood containing the antibodies, becomes separated from the blood cells. After further treatment, the serum is frozen, and will remain so until the arrival next month of Dr Robert Harrison, the head of the Alistair Reid Venom Research Unit at the Liverpool school. He will use new equipment worth Dh3 million (US$817,000) at CVRL to produce the antibodies needed for antivenom.
Once that is done, the antivenom will have to be tested, first on rodents and then on humans. Only then will it be ready for wider use. Then, according to Dr Wernery, the team will be ready for its next challenge - using the same technology to make camel-incubated vaccines for diseases such as polio, tuberculosis, malaria and even HIV. vtodorova@thenational.ae