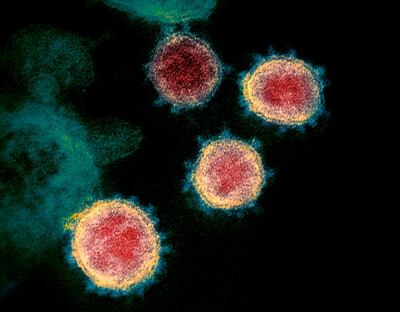
So far in 2020, Covid-19 has accounted for less than 1 per cent of deaths in Africa, even as widespread media coverage of the pandemic obscures other serious health emergencies. Malaria, alone, is 10 times more deadly. As of last week, a little over 53,000 recorded deaths in Africa have been linked to Covid-19. For comparison, the continent recorded 384,000 deaths due to malaria in 2019, as the World Health Organisation reported in its recent "World Malaria Report", released in late November.
Malaria is a preventable and treatable disease, and huge efforts have been made in the recent years; the very same report recounts that malaria deaths have reduced by 44 per cent over the past 19 years. Yet, our reactions to the coronavirus pandemic risk hampering these achievements and further exacerbating what is still a critical issue in Africa.
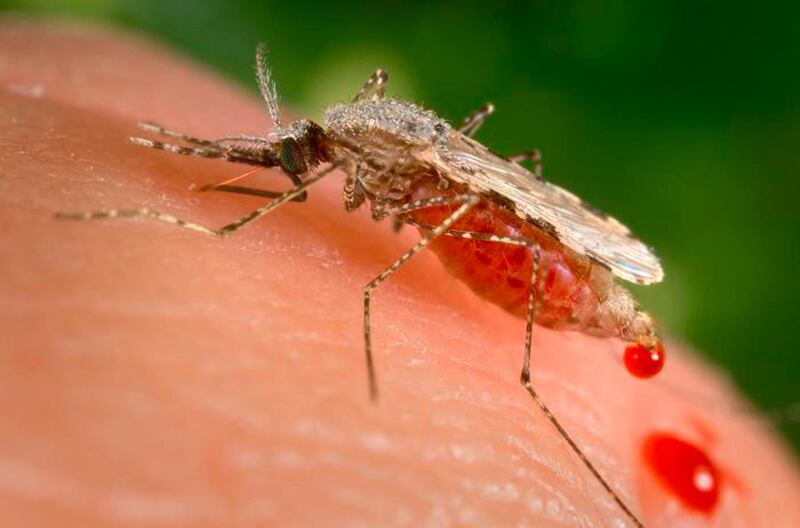
In the Sahel region, where our Doctors Without Borders (MSF) teams work, the peak of malaria struck more strongly and for longer this year. This is in part because the rains started earlier and were heavier compared to previous years, but also because national malaria prevention programmes have been impacted by the restrictions put in place in many countries across sub-Saharan Africa to stop the spread of Covid-19. Large-scale activities, such as mosquito net distribution and seasonal malaria prevention campaigns, have been slowed or postponed.
In Nigeria, the country with the highest number of malaria deaths in the world, the "Roll Back Malaria" partnership reported problems with regard to the supply of preventive treatment. These supply chain difficulties have already had consequences, including on the smooth running of seasonal prevention campaigns in the states of Borno and Kano where MSF teams are working. In Borno, the last round of the seasonal chemoprevention campaign, for instance, happened one month late. This risks losing the benefits of the first rounds, while access to health care is already very scarce there due to a conflict situation.
Globally, pharmaceutical production capacity has also shrunk in countries such as India and China, due to the pandemic and the restrictions put in place to control it. Some producers of rapid diagnostic tests for malaria – essential for quick and effective treatment – have started producing tests to diagnose Covid-19 instead, putting further strain on malaria projects. WHO also confirms that the supply of malaria medicines, including artemisinin-combination treatments, were particularly constrained because of hopes for a treatment to Covid-19. WHO analysis further suggests that even if malaria prevention campaigns are completed in 2020 as planned, disruptions to access to effective anti-malarial treatment could lead to considerable loss of life.
If we continue with this singular focus on Covid-19, the whole system – with its political, aid, economic and other players – risks actually contributing to the emergence of new health crises, with an even higher human toll. In Africa today, as tomorrow, the health and economic emergencies associated with Covid-19 are more the result of decision-making than the direct impact of the virus. Some of the disproportionate decisions are not made based on scientific evidence, but are driven by the fear generated by this virus.
For example, testing measures when entering a country have been shown to be more effective at the very start of an epidemic and when the virus is not circulating in the country. Implementing a lockdown once the epidemic is at the peak or when the virus’ circulation in a country is already out of control has not proved effective. When the virus is circulating in the country, priorities should rather focus on people at risk of dying from Covid-19 (those over the age of 65 years or with other illnesses, who certainly represent less than 10 per cent of the global population), rather than controlling or immobilising the entire working-age population of a country.
History will tell us the impact of these lockdowns on the global economy and the lives lost due to the economic precariousness they caused. Orienting healthcare systems mainly on Covid-19, which in the worst-affected countries represents less than 15 per cent of deaths, risks increasing casualties from other diseases because of a lack of access and thus creating a chain reaction leading to a burn-out of the health system. Another important element in any approach will be building relationships of trust with communities based on factual and scientific messaging, which contextualises deaths linked to Covid-19, particularly with regard to other public health issues.

In the many countries where Covid-19 is neither daily seen by the populations nor to be considered as one of the 10 leading causes of death by health authorities, it is time to rebalance public health priorities and treat Covid-19 as one disease among many.
With the year drawing to a close, the malaria peak in the Sahel is coming to an end, but other diseases will become a concern very soon. The performance drops in regular vaccination programmes seriously increase the risks associated with epidemics, such as measles, which are potentially more lethal than Covid-19 on this continent. Such risks are huge with preventive vaccinations having been delayed due to restrictions, but we will probably only be able to measure the impacts in the coming two or three years. In the shorter term, the rates of malnutrition will also be something to closely monitor, as the consequences of the pandemic are said to particularly risk increasing food insecurity in the coming months.
Dr Colette Badjo is the head of the MSF West and Central Africa office in Abidjan. Dr Dorian Job is the MSF West Africa programme manager