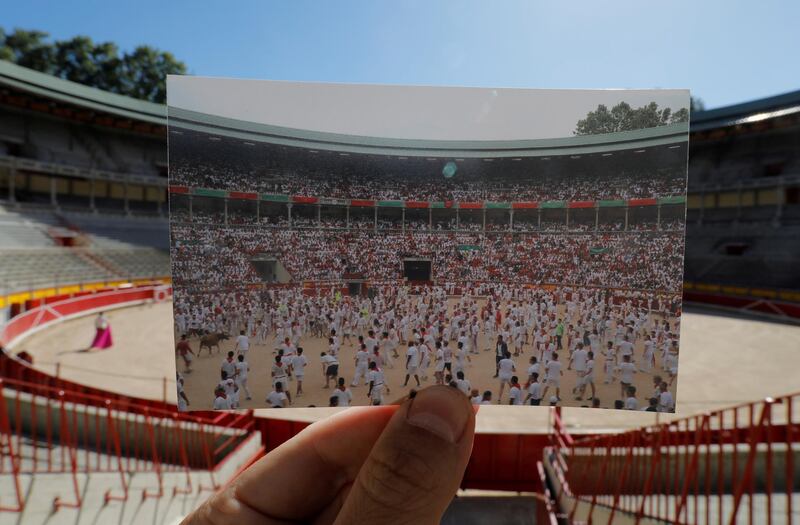
With daily cases of new infections worldwide hovering about 150,000, the need for an effective vaccine against the coronavirus is all too clear.
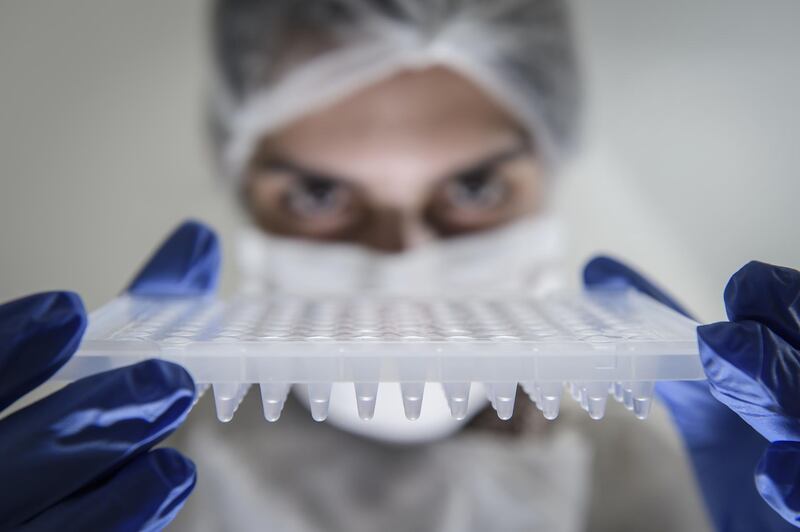
Hundreds of millions of dollars are currently being spent in support of 149 programmes globally, including trials in the UAE.
Pharmaceutical giants, small-scale biotech companies and universities are all behind the myriad of initiatives under way.
Cutting-edge techniques, together with more established research practices, are in the running, each with a singular focus on securing success.
In an interview with The National, Dr Andrew Freedman, an infectious disease specialist at Cardiff University in the UK, said there were significant benefits to having multiple research groups developing their own vaccines.
“It’s not clear at this stage which strategy will work,” he said. “If there was one perfect vaccine that could be produced in large enough quantities to supply the world, or however many people need to be vaccinated [that would be ideal], but vaccines are never perfect.
“It’s unlikely they will have a 100 percent effective vaccine, so the more the merrier. With various other infectious diseases there’s a choice of vaccines.”
To date, 19 vaccines from China, Germany, Russia, South Korea, the UK and the US have entered clinical trial stages.
Just one, developed by the UK’s University of Oxford with AstraZeneca, a British-based multinational pharmaceutical, has reached phase III trials, the final stage of testing before a vaccine can be licensed.
Described last month by WHO’s chief scientist, Dr Soumya Swaminathan, as “probably the leading candidate”, the Oxford vaccine is also the front-runner when it comes to the production of doses.
AstraZeneca has already signed multiple agreements with manufacturers to produce as many as two billion vaccinations annually, 400 million of which could be available as soon as this year.
The Oxford vaccine works by taking an existing, harmless version of the common cold virus and adding specific genetic material able to trigger an immune response known to help fight a Covid-19 attack.
But there are significant question marks over its effectiveness. The vaccine prevented serious illness in monkeys, but left the animals with large quantities of the virus in their nasal passages.
The journal Nature has also reported similar concerns about an advanced Chinese vaccine programme involving the pharmaceutical company Sinovac.
Inside Abu Dhabi Stem Cell Centre for coronavirus treatment

Its vaccine – which is in phase I/II clinical trials – is based around an inactivated form of the coronavirus, meaning the virus has been treated with heat or chemicals to prevent it being able to infect human cells.
“The landscape has changed considerably over the last six weeks,” said Ian Jones, a professor of virology at the University of Reading in the UK.
“The data that’s available is mixed. For the Oxford vaccine, the protection [appears to be] against disease, but not against infection.”
Professor Robin Shattock, who heads the UK’s other coronavirus vaccine programme at Imperial College London, urged caution when attempting to interpret animal trials.
“Clearly you want a vaccine that prevents transmission more than one that just prevents severe disease,” he said.
“But if a vaccine comes along that prevents severe disease, that would still have utility in a very vulnerable population.”
Another front-running vaccine, from the American biotechnology company Moderna, is due to enter phase III clinical trials later this month.
It has a less tried-and-tested approach, being based on a type of genetic material known as messenger RNA (mRNA).
The mRNA causes human cells to produce a protein that stimulates an immune response that protects against the coronavirus.
While the value of Moderna’s stock has swelled to tens of billions of dollars in recent months, the company is known for its secrecy and has not released full data about its early trials.
Significantly, no RNA vaccine, which have proved effective in the treatment of animals, has yet been licensed for use in people, despite more than a decade of research.
While the race to produce the world’s first effective vaccine has invariably attracted much attention, the earliest product to be licensed may not be the one that ends up dominating the market.
Indeed, with so many vaccines in development, it is perhaps more likely that a later product will prove the most effective.
“As we learn more about the individual candidates, the ones that give the best and the highest level [of protection] for the longest period, even if they’re introduced later, they will start to dominate the field, depending on the cost,” said Prof Shattock.
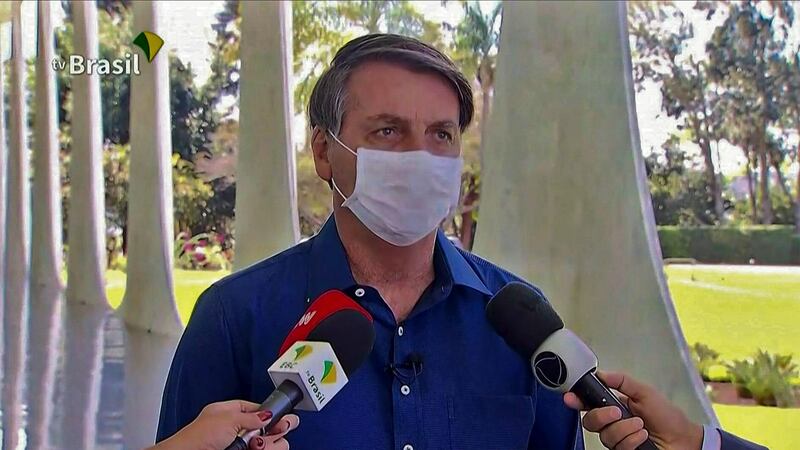
Trump: 'I told officials to slow coronavirus testing down'

“The chances that none will work is low. It may be [there’s] a few that work and it’s dangerous to predict a level of certainty."
Prof Shattock went on to outline how it was likely to prove difficult for one vaccine, when ready, to be produced in sufficient quantities to satisfy global demand.
A vaccine that is particularly expensive may be unaffordable to poorer economies, although it is hoped single doses of some vaccines may cost as little as a few dollars.
Another factor favouring the eventual use of multiple vaccines is that certain types may prove more effective within set populations.
“It may be that one vaccine works better in children, another works better in older people,” said Dr Freedman.
“There may be safety issues; one has more side effects in particular age groups or immunocompromised groups.”

So how much longer will it be before a vaccine becomes licensed and large-scale production starts?
This could happen late this year for, among others, the Oxford and Moderna vaccines, as well as one or more of the multiple Chinese vaccines.
However, given the scale of the demand, early supplies may be given only to particular groups, such as the over 55s and healthcare workers, Prof Jones suggested.
“I don’t think we will see significant amounts available in the global market before the middle of next year,” he said.
The Imperial College vaccine programme
No vaccine made from RNA, a type of genetic material, has yet been licensed for use in people.
Yet despite this, there are now 20 separate programmes in the process of developing the complex nucleic acid to help combat the new coronavirus.
The ongoing work at Imperial College London is based on RNA that is encapsulated in a fat droplet and injected into arm muscles.
Once delivered into a person, the RNA causes human cells to produce a protein that stimulates an immune response that should protect against Covid-19.
“The relative advantage of the approach is, first of all, it’s quick to design and manufacture,” said Professor Robin Shattock, who heads the programme.

“The second is that we can use a very low dose to induce what we predict will be a preventative immune response, much lower than what other RNA companies are proposing to use – about 100 times lower.
“So in terms of scalability you have this advantage, and in terms of cost.”
Prof Shattock said it should be clear by early next year as to whether the Imperial College vaccine produced a suitable immune response without significant side effects.
There is already capacity to produce enough of the vaccine for the UK, but additional partnerships would need to be struck to supply other parts of the world. A key aim is to ensure its availability for developing nations.
“If the vaccine works and lots of people wanted it, I think there would be lots of funding available to produce it,” said Prof Shattock.
“It would start in the UK in the first two quarters [of 2021]. When it could start in other parts of the world depends on when any commitment was made to fund the manufacture of these other doses.”