We've all done it. Faced with some malfunctioning gadget or computer, we pull the plug on it, switch it back on - and find it works perfectly again. Known to the cognoscenti as the "hard reboot", it's a trick used more often in desperation than insight. Now it's emerging as a promising new approach to treating some notoriously debilitating medical conditions. Recent clinical trials have shown that "rebooting" our disease-fighting immune system can dramatically improve the condition of patients with multiple sclerosis and rheumatoid arthritis. And according to a study published last week, it may even bring relief to patients suffering from the enigmatic condition Chronic Fatigue Syndrome, affecting millions worldwide.
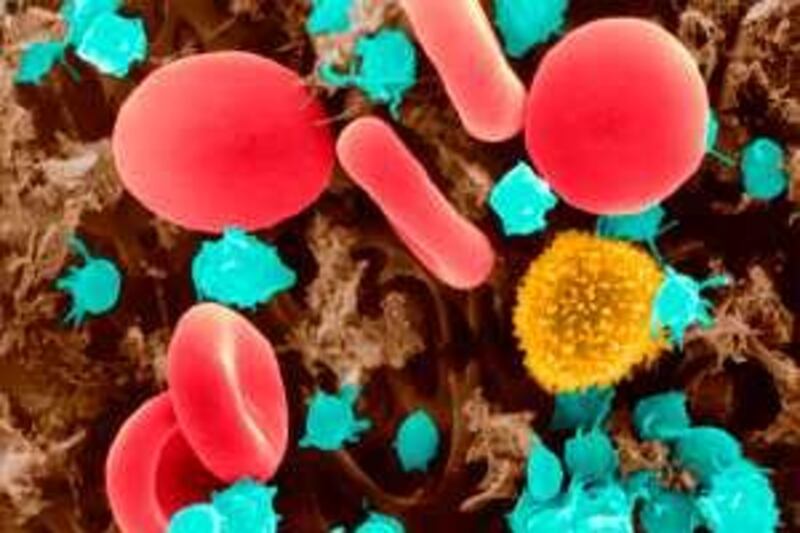
There is a growing sense of excitement about the rebooting technique. But behind it lies an inspiring story of how a pair of scientists overcame indifference to convince the medical community of the merits of what is now called B-cell Depletion Therapy (BCDT). B-cells are a type of white blood cell which randomly churn out so-called antibodies, many of which prove useful in destroying disease-causing pathogens. Yet, like every defence system, mistakes sometimes happen - and innocent bystanders end up being targeted. During the late 1990s, two medical researchers at University College London began to wonder if this "friendly fire" might hold the key to the debilitating disease rheumatoid arthritis (RA).
Affecting about one in 100 people worldwide, RA can strike anyone literally overnight, their immune system suddenly attacking their joints. The condition is excruciatingly painful, and for years there seemed no hope of a cure. Until recently, the prime culprit was held to be T-cells: white blood cells that play a key role in the disease-fighting immune system. Yet despite intensive study, no one could explain how or why T-cells should produce a lifelong ailment such as RA. Most tellingly of all, therapies targeting T-cells failed to benefit patients.
This prompted Professor Jonathan Edwards and Dr Geraldine Cambridge at UCL to ponder the possibility than B-cells might be to blame. Their idea was based on the fact some B-cells are known to make antibodies which inadvertently seek out and destroy healthy tissue. Normally, these would be destroyed by the B-cells themselves. But what if some of the antibodies by chance possessed the means to evade their own destruction - and go on to attack the joints?
That led Prof Edwards and Dr Cambridge to a radical new approach to treating RA: "rebooting" the immune system by destroying all the B-cells, and then starting over with fresh ones. Fortunately, a compound capable of targeting just B-cells had just become available: rituximab, a so-called monoclonal antibody which homes in on specific targets like a heat-seeking missile. This could destroy all the B-cells, leaving patients to develop a whole new set free of the renegade variety that attack joints.
That at least was the theory, and with the standard T-cell theory not getting anywhere, the team thought it was worth bringing to the attention of other researchers. They soon found that new ideas aren't always welcome in science - even if the old ones aren't working. Their academic papers were rejected by journals as "obviously" wrong - on the grounds that they focused on B-cells, not T-cells. They were not helped by a lack of experimental evidence. Yet the pair found themselves in a chicken-and-egg scenario: only if they already had evidence from clinical trials could they persuade funding bodies to pay for more clinical trials.
The pair managed to publish their idea in a medical journal, only to be met with silence. Determined to make their case, they set up a small but demanding test, using rituximab to treat five patients with severe RA. The results were impressive: once their B-cell systems had been "rebooted", their condition improved dramatically. Yet attempts to publish the results in journals were rebuffed on the grounds that the study involved too few patients.
So the pair tried again, cobbling together enough money to treat 20 patients. Again, the results were impressive, with all but two of the patients showing dramatic improvements. It made no difference: the medical community remained utterly unimpressed. Frustrated by the lack of interest, Prof Edwards and Dr Cambridge decided some media coverage might help. When the reports of their success with 20 patients emerged, they found themselves vilified by fellow academics as hype-mongers.
Whatever the rights or wrongs of their decision to approach the media, it certainly boosted awareness of the B-cell depletion theory. In 2000, just six people had turned up to hear a lecture about the theory; a few months later, the media coverage led to 3,000 packing a lecture hall to hear what it was all about. The coverage also helped win funding for a substantial clinical trial involving more than 160 patients. By 2002, the results were in: when combined with a standard therapy for RA, rituximab proved three times more effective than the standard therapy alone. In 2006, the B-cell depletion therapy (BCDT) was approved by regulators in the US and Europe for use alongside the standard therapy.
Despite this vindication, the two researchers have not rested on their laurels. Since the late 1990s, they have suggested that BCDT might help in treating another disease linked to a malfunctioning immune system: multiple sclerosis. Last year, a study of more than 100 patients showed that BCDT could halve their relapse risk. The UCL team has also shown that the technique brings benefits to patients with the auto-immune disease, lupus.
Now a team of researchers in Norway is claiming the therapy could help treat Chronic Fatigue Syndrome, sometimes called myalgic encephalomyelitis (ME). Characterised by mental and physical exhaustion, with muscle and joint pain, this enigmatic condition has no accepted cause. Many researchers have suspected a link with the immune system - a possibility now tentatively backed by researchers at Haukeland University Hospital, Norway. In the current issue of the online journal BioMed Central- Neurology, the team reports treating three CFS patients with BCDT, and observing marked improvements.
With so few patients, it's hardly definitive proof of a cure. Yet it is just the situation Prof Edwards and Dr Cambridge found themselves in a decade ago. CFS sufferers must be hoping medical researchers are not about to repeat history by rejecting these intriguing findings out of hand - despite not having any better ideas themselves. Robert Matthews is a Visiting Reader in Science at Aston University, Birmingham, England